What is the biopsychosocial model of healthcare?
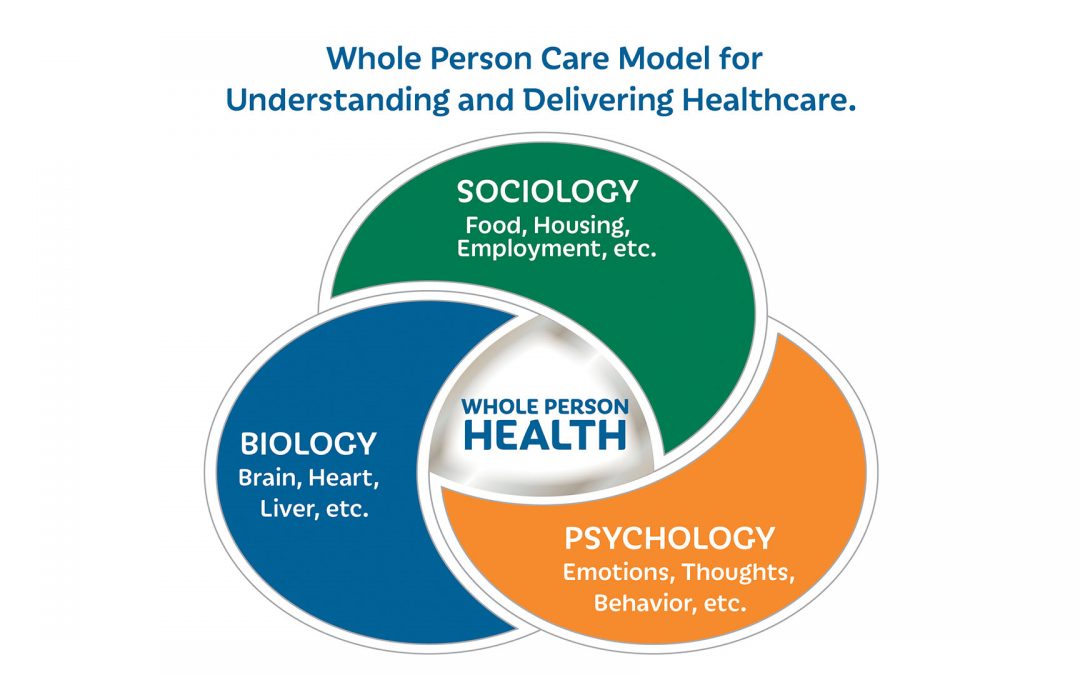
The biopsychosocial model of healthcare is both a concept for understanding health, disease, and illness, and a framework for delivering healthcare.
The foundational belief of the biopsychosocial model is that one’s biology, psychology, and sociology all have to be considered when delivering healthcare. Often all three elements have to be addressed together in order for healthcare delivery to be effective. This is particularly important for those suffering with chronic medical conditions (e.g., diabetes, COPD), chronic pain, functional illnesses (e.g., IBS, chronic fatigue, fibromyalgia), and brain illnesses (e.g., bipolar, schizophrenia, depression, anxiety, and substance use dependency).
What is whole-person care?
Healthcare providers and healthcare delivery systems committed to a biopsychosocial model often use the term “whole-person” when describing their healthcare model. And “whole-person care” is a term that captures the essence of the biopsychosocial model. Whole-person healthcare providers respect the interconnectedness of a patient’s body (all of one’s organs, including the brain), a patient’s psychology (one’s feelings and thoughts). and a patient’s living environment. That interconnectedness affects health outcomes.
Whole-person healthcare reflects the understanding that each person is unique, with unique responses to disease, illness, substance use, and societal challenges. There is no-one-size-fits all approach to caring for a patient. The model also reflects an understnding that healthcare must be delivered without any moral judgment or stigmatization by providers or society.

Biology
In the context of the biopsychosocial model, biology refers to the influences and interplay of genetics, physiology, anatomy, epidemiology, and nutrition on the organs of the body.

Psychology
In the context of the biopsychosocial model of care and the whole-person care model, psychology refers to an individual’s feelings, thoughts, and behaviors.

Sociology
Sociology refers to how individuals live in a social context; how they relate to themselves, family, social groups, and society; whether they have financial security and a sense of safety, and how socio-cultural influences impact their health. These variables are all factors of social determinants of health.
Primary care and the biopsychosocial model of care
Primary care providers are usually the first contact for individuals with undiagnosed health concerns. Providers need to diagnose and address a wide range of health problems, both acute and chronic. While some patients present with diseases that can be detected with biomedical tests that lead to concrete treatments, other patients present with symptoms that tests cannot detect. In these cases, patients may have no organic evidence that can readily explain symptoms. This is often true of chronic fatigue, chronic pain, fibromyalgia, brain fog, and brain disorders, among other illnesses.

When patients do present with undiagnosable symptoms, providers using a biopsychosocial model of care validate their patients’ symptoms. They know that a patient does not need to have a biomedical diagnosis to have an illness. They can approach treatment options from different angles. The biopsychosocial model is therefore a model that follows both science and a broader, humanistic approach in its delivery, respecting patients’ experience of illness and validating their feelings and explanations about symptoms. The model also encourages patients to play an active and responsible role in their healthcare whenever possible.
This multidisciplinary approach to addressing a patient’s needs is ever watchful of the interplay among the biological, psychosocial, and sociological components of illnesses. When used effectively, the biopsychosocial model can improve clinical outcomes for chronic disease, functional illnesses, and brain health disorders seen in primary care.
Brain illnesses and the biopsychosocial model of care
The biopsychosocial model of care also recognizes that illnesses of the brain (depression, anxiety, bipolar, autism, schizophrenia, and other brain diseases and disorders) are as “biological,” “real,” and “legitimate” as organ illnesses such as cancer, diabetes, and ulcers. Brain illnesses always require a whole-person approach, and providers always advocate for rejection of any form of stigmatization or moralistic judgments that are harmful to patients with any form of brain illness or disease.
Primary care providers serving patients with brain illnesses using a whole-person approach appreciate how brain illnesses impact all aspects of an individual’s ability to live their healthiest and safest life.
Skilled providers also know that there is wide variability in how patients experience brain diseases just as there is with other bodily chronic illnesses and diseases. Therefore, treating a patient as a whole person, and attending to a patient’s unique biology, psychology, and social situation is critical to achieving the best outcomes for that individual patient as well as for their families and the community around them.
The biopsychosocial/whole-person model in the U.S. Healthcare System
The three domains considered important in the biopsychosocial model–biology, psychology, and social determinants of health–are too often functionally separated within the United States health systems due to both conceptual and reimbursement structures. However, as health care clinicians have become increasingly aware of the importance of brain health and the role psychological factors and social determinants of health play in a patient’s overall health, it is increasingly critical that health systems reevaluate their delivery of care in order to achieve better health outcomes and long-term health cost savings.
Catawba Valley Healthcare practices a whole-person model of healthcare
At Catawba Valley Healthcare (CVH), we believe in, and practice, a whole-person model of health care in our primary care clinic and brain health services. We deliver whole-person healthcare in order to deliver optimal care for our patients. We fully recognize that each patient has unique needs. We believe in interprofessional collaboration between our primary care providers, brain health care providers, and social workers whenever necessary to address the biological, psychological, and social health aspects of healthcare delivery. And we respect the personal, familial, and cultural differences of all our patients.
In many healthcare systems, coordination of care can be difficult and time-consuming as patients wait for different providers to communicate with each other. CVH and our providers wanted to change that. At CVH, both brain health and primary care providers work together under one roof towards one goal: integrated patient care. We take the biopsychosocial, whole-person model of care seriously in order to practice what we believe is the best model for healthcare delivery for all of our patients.
For more information on all of Catawba Valley Healthcare services, visit our website: cvhnc.org
Biology

Psychology

Sociology
Sources:
- J Family Med Prim Care. 2018 May-Jun; 7(3): 497–500. Biopsychosocial model of illnesses in primary care: A hermeneutic literature review. Hari Kusnanto, Dwi Agustain, and Dany Hilmanto.
- Jama Psychiatry, June 3, 2020. Psychosocial Factors in Disease and Treatment–A Call for the Biopsychosocial Model. Veronika Engert, PhD, Joshua A. Grant, PhD, Bernhard Strauss, PhD.