HELP and HOPE
As you read this blog about Serious Mental Illness (SMI), please remember that there is help and hope for EVERYONE with a mental illness, including those with SMI. In fact, our motto at Catawba Valley Healthcare (CVH) is “Where Help and Hope Meet.” We are dedicated to providing effective evidence-based treatment for everyone who comes to us for help. Through counseling, peer support, medication management, and a variety of other supports, help is available for you or your loved one.
What is a Serious Mental Illness (SMI)?
A Serious Mental Illness (SMI) is a mental health diagnosis that creates substantial functional impairment in at least one life activity such as work life, family life, or community life. For example, someone with Schizophrenia or Bipolar Disorder may have difficulty coping and functioning in everyday life due to wide mood swings or challenges understanding the world around them. Although SMI’s are serious health conditions, with treatment and support from friends, family and their communities, people with SMI often experience remarkable improvement in their quality of life and decrease in their symptoms. At CVH, we think of “mental illness” as a reflection of brain health. The brain “controls your moods, emotions, behaviors, decision-making, and more.” As a result, we “strive to eliminate any and all fear, shame, embarrassment, or misconceptions that individuals may feel in seeking health care for their brain/mental health. There should never be any stigma around caring for this essential organ.” The importance of brain function is especially true for SMI’s, which often are related to various changes or malfunctions in brain chemistry.
Types of Serious Mental Illness and Their Symptoms
Some of the most frequently diagnosed SMI’s include Schizophrenia, Bipolar Disorder, Borderline Personality Disorder, Major Depressive Disorder, Anxiety Disorders, and Post Traumatic Stress Disorder. Selected symptoms of some of the most common serious mental illnesses are shown in the table below. It’s important to remember that the intensity or severity of symptoms, as well as how long they have persisted, often determine whether a particular diagnosis is made. Also, in some cases, additional symptoms may be required for the diagnosis to be made. Some individuals have more than one SMI, and many people with SMI also have a Substance Use Disorder. In fact, the Substance Abuse and Mental Health Administration (SAMHSA) reports that in 2020 2.2% of adults aged 18 and older had both an SUD and an SMI (see page 3 of Key Substance Use and Mental Health Indicators in the United States: Results from the 2020 National Survey on Drug Use and Health).
| Condition | Select Symptoms* |
| Schizophrenia | Delusions (false beliefs), hallucinations (seeing or hearing things that don’t exist), unusual physical behavior, and disorganized thinking and speech |
| Bipolar Disorder | Unusual shifts in mood, ranging from extreme highs (mania or “manic” episodes) to lows (depression or “depressive” episode). Changes in energy, thinking, behavior, and sleep. Difficulty carrying out day-to-day tasks, going to work or school, and maintaining relationships. Manic episodes may include excessive energy, speaking fast or being unusually talkative, racing or jumbled thoughts, distractibility, or inflated self-esteem. Depressive episodes may include feeling sad or hopeless, forgetfulness, indecisiveness, difficulty concentrating changes in appetite, or thoughts of death or suicide. |
| Major Depression | Persistent feelings of sadness, hopelessness, or emptiness; Fatigue; Too much or too little sleep; Loss of interest in pleasurable activities; Anxiety or irritability; Feeling worthless; Weight loss or gain; Moving, talking, or thinking more slowly; Forgetfulness; Trouble concentrating, thinking clearly, or making decisions; Suicidal thoughts or attempts or other self-harm behaviors |
| Post Traumatic Stress Disorder | Flashbacks, Trouble sleeping or nightmares, Feeling alone or detached from others, Losing interest in usual activities, Angry outbursts, Feeling worried or guilty or sad, Having frightening thoughts, Trouble concentrating, Physical pain like headaches or stomach aches, Avoidance of memories, thoughts, or feelings about traumatic events, Problems remembering, Negative beliefs about themselves or others, Irritability, Feeling very vigilant, Startling easily |
| Borderline Personality Disorder | Uncertainty about one’s identity, Rapidly changing interests and values, Things are viewed in extremes, Intense and unstable relationships, Intense fear of abandonment, Cannot tolerate being alone, Frequent feelings of emptiness, Frequent inappropriate anger, Impulsive and risky behavior, Repeated crises and acts of self-harm, Distorted sense of self |
| * Symptoms are adapted from information at www.Samhsa.gov and not all symptoms are listed. | |
Table 1: Selected Symptoms of Common SMI’s

Mental Illness vs. Serious Mental Illness: Understanding the Difference
Many SMI’s have similar characteristics to less serious mental illnesses, but they are more extreme and/or cause more impairments to daily living. For example, think of three people who are “feeling sad.” One may be disappointed and feeling sad because he experienced problems at work or broke up with his partner, but he may be functioning as usual at home, work, and other community activities, other than occasional mild problems getting to sleep and occasional periods where he feels like crying. That person may simply be “sad.” Someone else may have experienced a major loss, such as the death of a loved one, or being fired from her job. This person may be struggling to cope with job interviews, may be losing her temper occasionally, and sometimes may have difficulty sleeping, but overall still coping with most tasks and responsibilities of daily living. This person may be diagnosed with Adjustment Disorder with Depressed Mood, which is a mental illness, but usually not considered an SMI. The third person may have periods of deep sadness that prevent him or her from working, may have significant sleep problems, may have distorted or psychotic thinking, and may have suicidal thoughts or attempts. These symptoms definitely impair the person’s ability in at least one major life activity. That person may be diagnosed with Major Depression, which is an SMI.
All three people experience sadness and some difficulties with sleep, as well as differences in severity and duration of their symptoms, but only one of them has an SMI. Similar examples could be given for SMI’s like Schizophrenia or Bipolar Disorder, which are similar in some ways to less serious mental illnesses, such as Schizotypal Personality Disorder or Cyclothymic Disorder. Individuals with Schizotypal Personality Disorder have difficulty with relationships and may have somewhat distorted perceptions of reality, but not to the same degree as someone with Schizophrenia. People with Cyclothymic Disorder have mood swings and may use poor judgment, but not to the same extent as someone with Bipolar Disorder.
Prevalence of SMI in the United States
According to the National Institute for Mental Health (NIMH), in 2021 there were 14.1 million adults in the U.S. who had an SMI. Those 14.1 million people represent 5.5% of the U.S. adult population. The prevalence was 7% for females and 4% for males. In general, the prevalence of SMI decreases for older age groups, with the highest prevalence among adults 18 to 25 years old (11.4%) and the lowest among adults 50 and older (2.5%). Although children also can be diagnosed with an SMI, in general, SMI is not diagnosed until adulthood. Consequently, for children, prevalence is usually reported for mental illness but not for SMI. For example, in 2016 the American Academy of Family Physicians estimated that about 17% of children had a diagnosable mental illness, such as depression, attention-deficit/hyperactivity disorder, or anxiety disorder.
The Impact of SMI on Families and Society
The effects of SMI on family members and the community are numerous. For families, the mental illness of one family member can impact the emotional and financial wellbeing of the entire family. Individuals with SMI often have one or more family members who serve as a caregiver or who are affected in numerous other ways. Think of the effects on a family of a person with Bipolar Disorder who might binge on alcohol, or who might be in a manic phase where he or she suddenly decides to paint the entire house and stays up all night trying to do so. Or, think of the effects on a family of someone with Post Traumatic Stress Disorder who goes through periods of intense depression, with thoughts of suicide, or has intense nightmares where he or she wakes up screaming in the middle of the night.
Think of the family of anyone with an SMI who might need hospitalization for a period of time, and how that decision may affect the entire family. There are endless examples of how each family member is affected by the illness of the person with an SMI. At the same time, when family members pull together to understand and support the individual with an SMI, it can be a powerful and meaningful experience for everyone in the family. Remember, there is “help and hope” and it is often family members who help their loved one with an SMI access that help and hope.
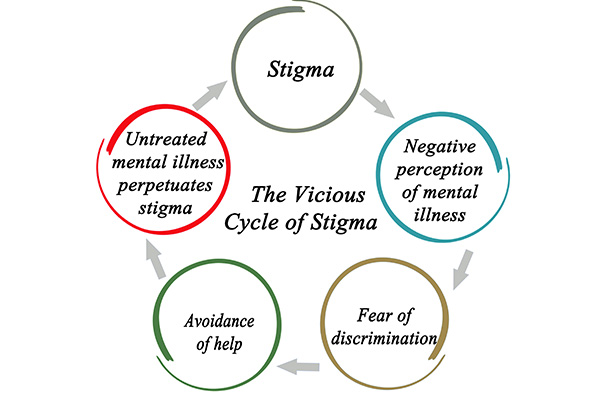
Communities are also affected by SMI, both economically and in terms of quality of life. For example, according to a report released in May 2022 by the White House, mental health treatment in the U.S. cost about $280 billion. Although these costs are high, it’s important to remember that many people who would benefit from treatment don’t receive it, often because they can’t afford it, because of the perceived stigma, or because they don’t have convenient access. At CVH, we believe that the cost to society of providing mental health treatment should be viewed as an investment in the health of those treated, as well as the overall quality of life of communities.

Treatments for SMI
The most common forms of treatment for SMI’s include psychotherapy and medication management. Medications prescribed to treat mental health symptoms are usually called psychotropics and typically include antipsychotic medications, antidepressants, anti-anxiety medications, mood stabilizers, and stimulants. In many cases, both psychotherapy and medication management are appropriate. Other treatment options include family therapy, various forms of care management, peer support, and day treatment programs, sometimes called psychosocial rehabilitation. Treatment for SMI also sometimes includes periods of hospitalization, usually for the purpose of medication adjustment and stabilization, and sometimes to protect the safety of the individual or others if he or she is having suicidal or homicidal thoughts or intentions. Treatment starts with a thorough and respectful evaluation in order to determine a correct diagnosis and a helpful treatment plan that reflects the strengths, needs, goals, and preferences of each individual.
Additional Information
The links below include recommended sites that include information about the causes and common symptoms of mental illness, the importance of family and social support, the impact of mental illness on society, the impact of stigma, effectiveness of treatment, recovery, the prevalence of Substance Use Disorder and SMI, and much other useful information:
- American Psychiatric Association (APA): https://www.psychiatry.org/patients-families/stigma-and-discrimination
- Centers for Disease Control and Prevention (CDC): https://www.cdc.gov/mentalhealth/learn/index.htm
- National Institute on Drug Abuse: https://nida.nih.gov/publications/research-reports/common-comorbidities-substance-use-disorders/part-1-connection-between-substance-use-disorders-mental-illness#:~:text=Around%201%20in%204%20individuals%20with%20SMI%20also%20have%20an%20SUD.&text=Data%20from%20a%20large%20nationally,nonmedical%20use%20of%20prescription%20opioids.
- National Institute of Mental Health (NIMH): https://www.nimh.nih.gov/health/statistics/mental-illness#:~:text=Prevalence%20of%20Serious%20Mental%20Illness%20(SMI),-Figure%203%20shows&text=In%202021%2C%20there%20were%20an%20estimated%2014.1%20million%20adults%20aged,5.5%25%20of%20all%20U.S.%20adults
- Substance Abuse and Mental Health Administration (SAMHSA): https://www.samhsa.gov/serious-mental-illness
- Turnbridge: https://www.turnbridge.com/news-events/uncategorized/untreated-undiagnosed-mental-illness/
- Veterans Affairs (VA): https://www.mentalhealth.va.gov/communityproviders/wellness-smi.asp
- World Health Organization (WHO): https://www.who.int/news-room/fact-sheets/detail/mental-disorders
This blog was authored by Donald W. Mott, LPA